Parasite Testing at DSHS Laboratory
|
The DSHS Laboratory does not accept parasitology specimens from the public. Only healthcare providers can order parasitology tests and submit specimens for testing. Specimens submitted by the public will be rejected and destroyed. If you believe you have a parasitic infection, please talk with your healthcare provider. Laboratory staff cannot provide medical advice. Your provider will contact the DSHS Parasitology Laboratory for specimen submission requirements, if needed. |
- Parasitology Home | Parasite Testing at DSHS Laboratory | Refugee Health Testing | Submitting Parasitology Specimens to DSHS | Parasitology FAQs | Parasitology Resources
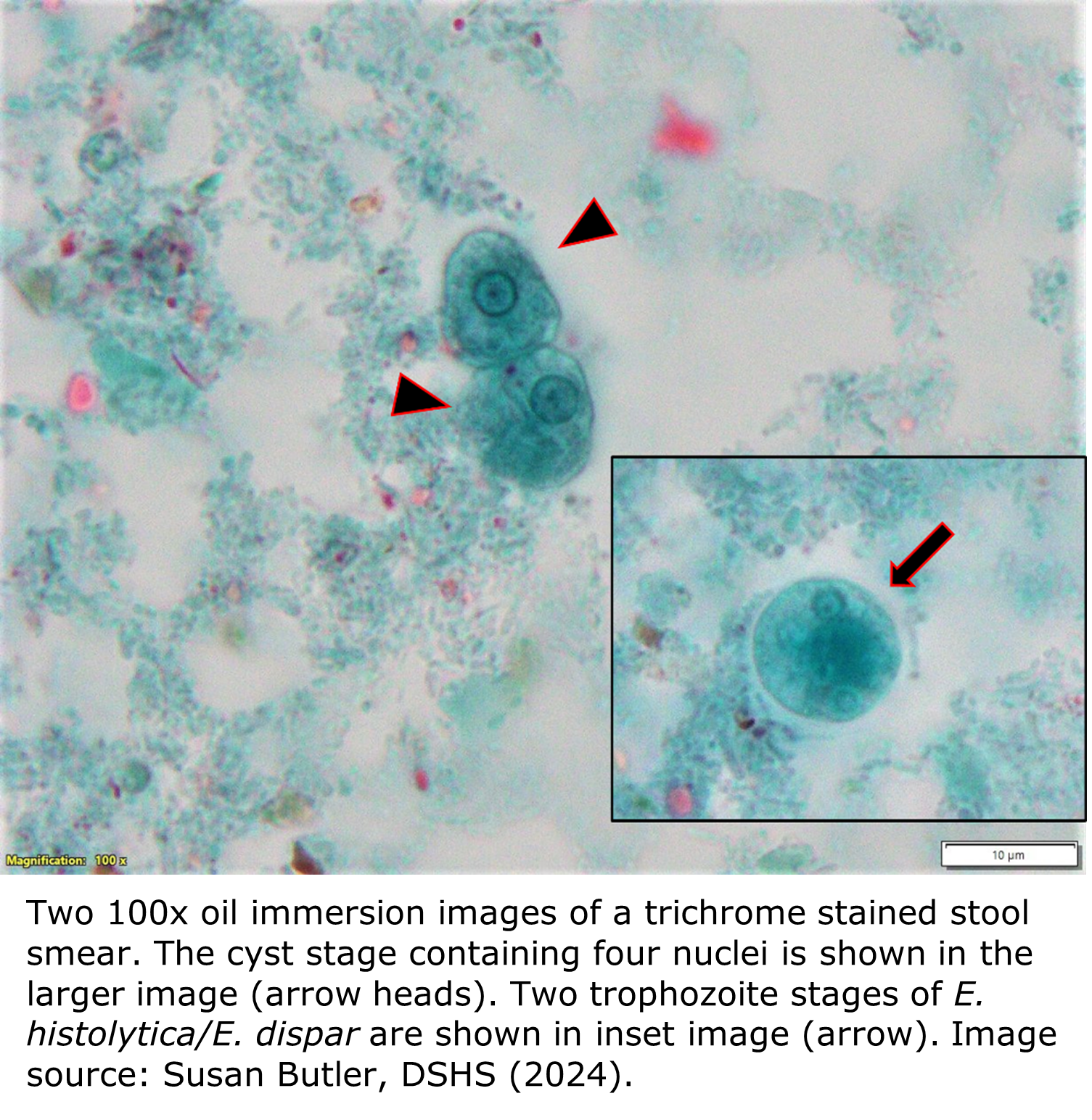
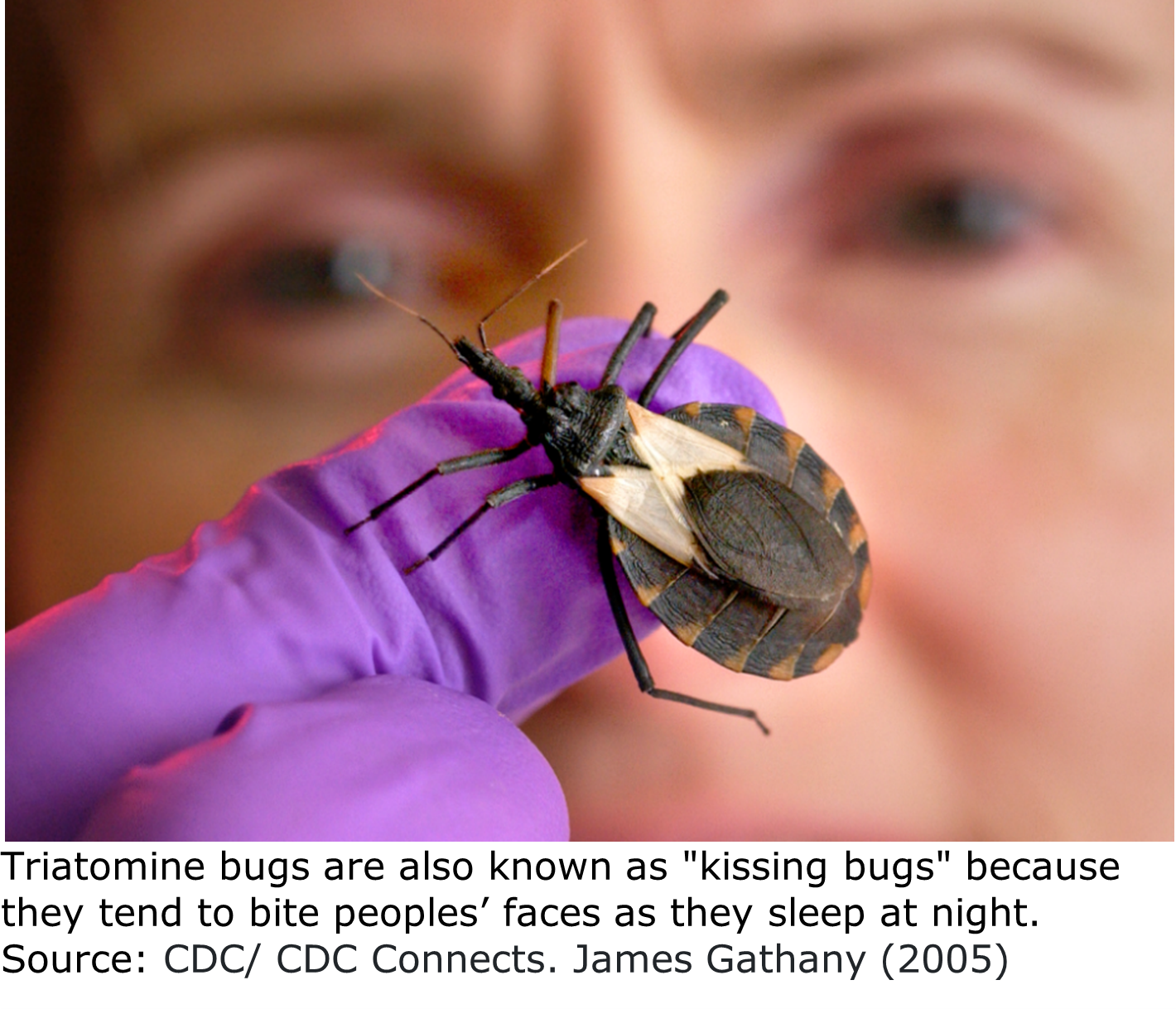
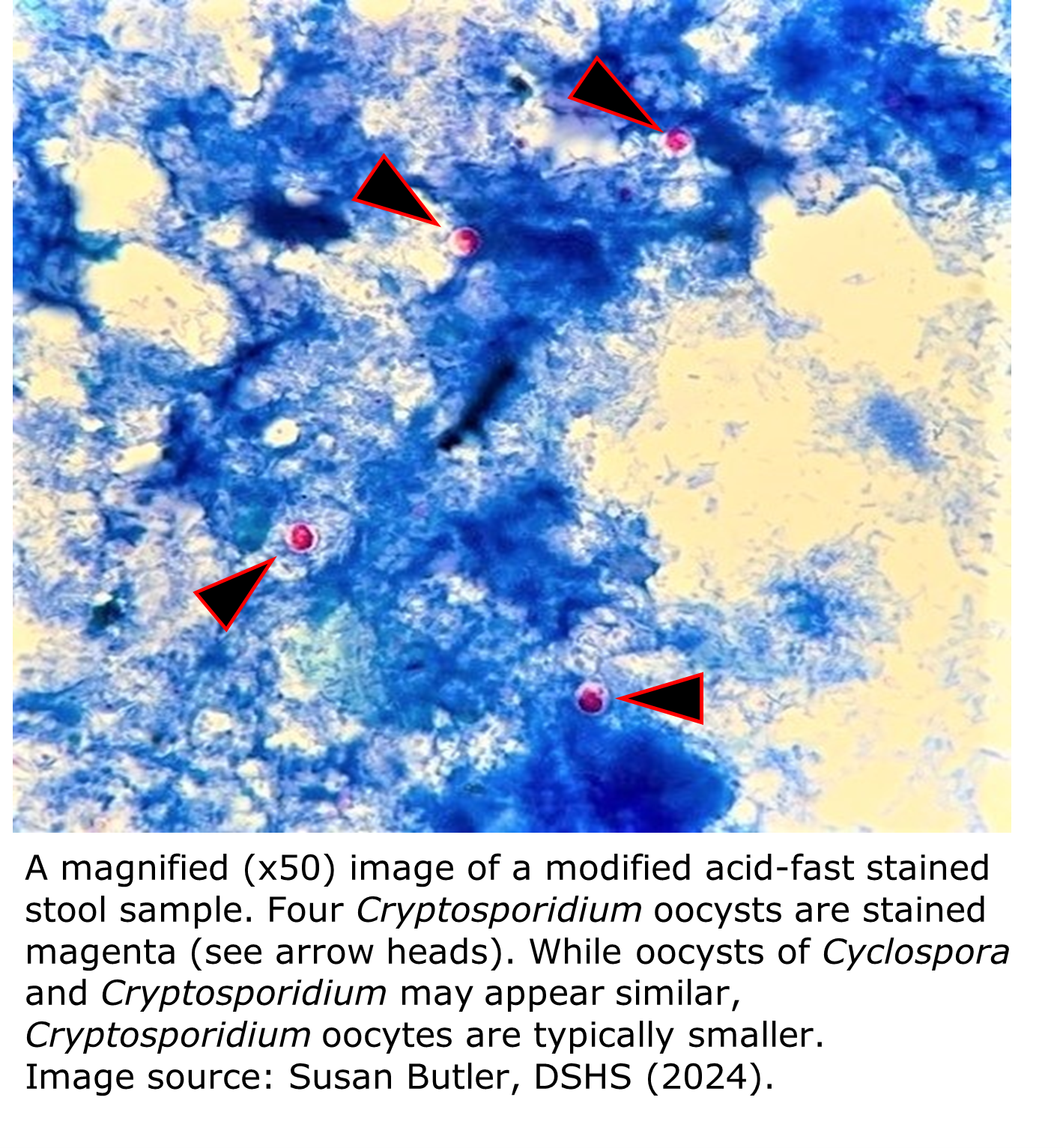
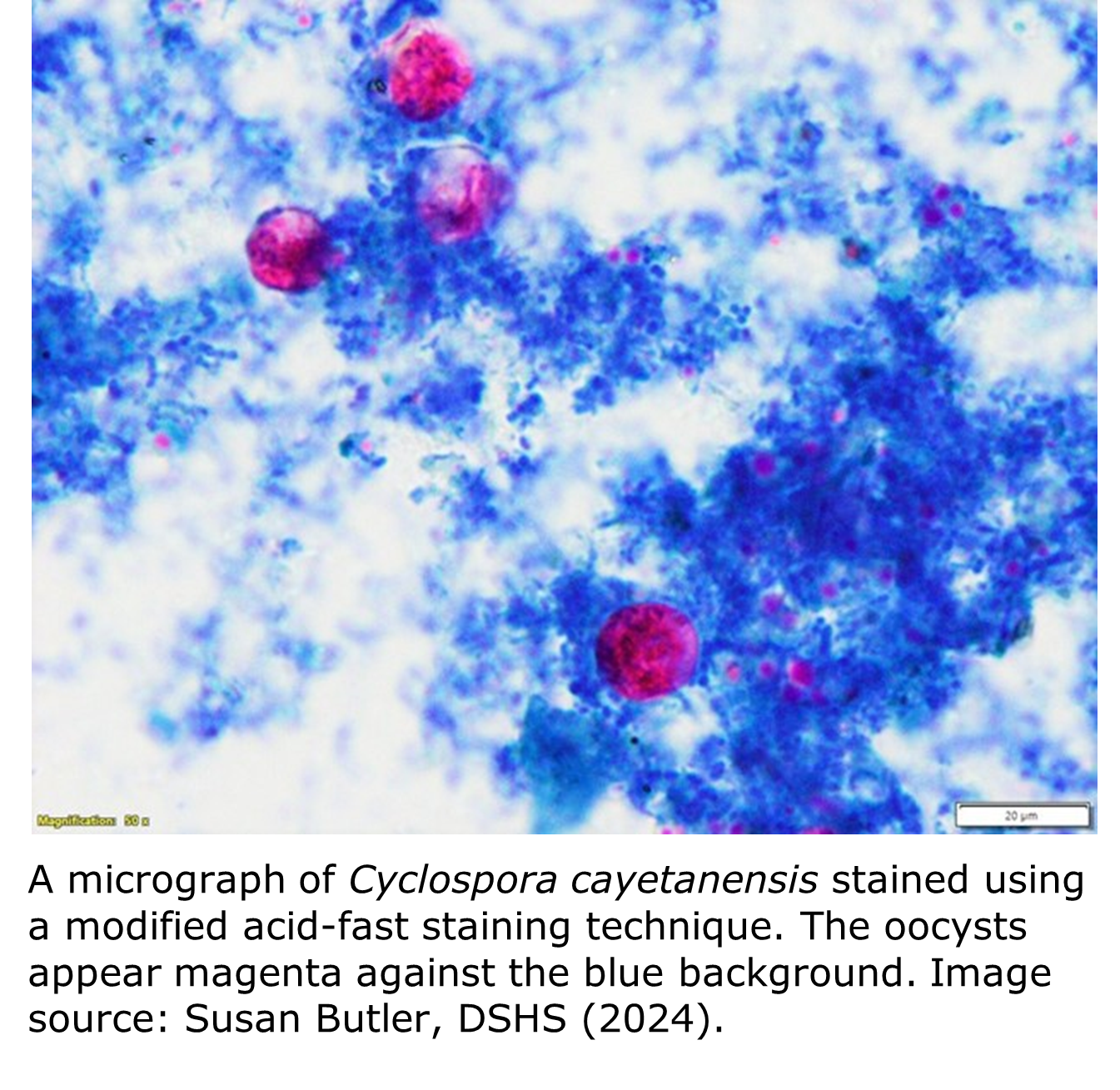
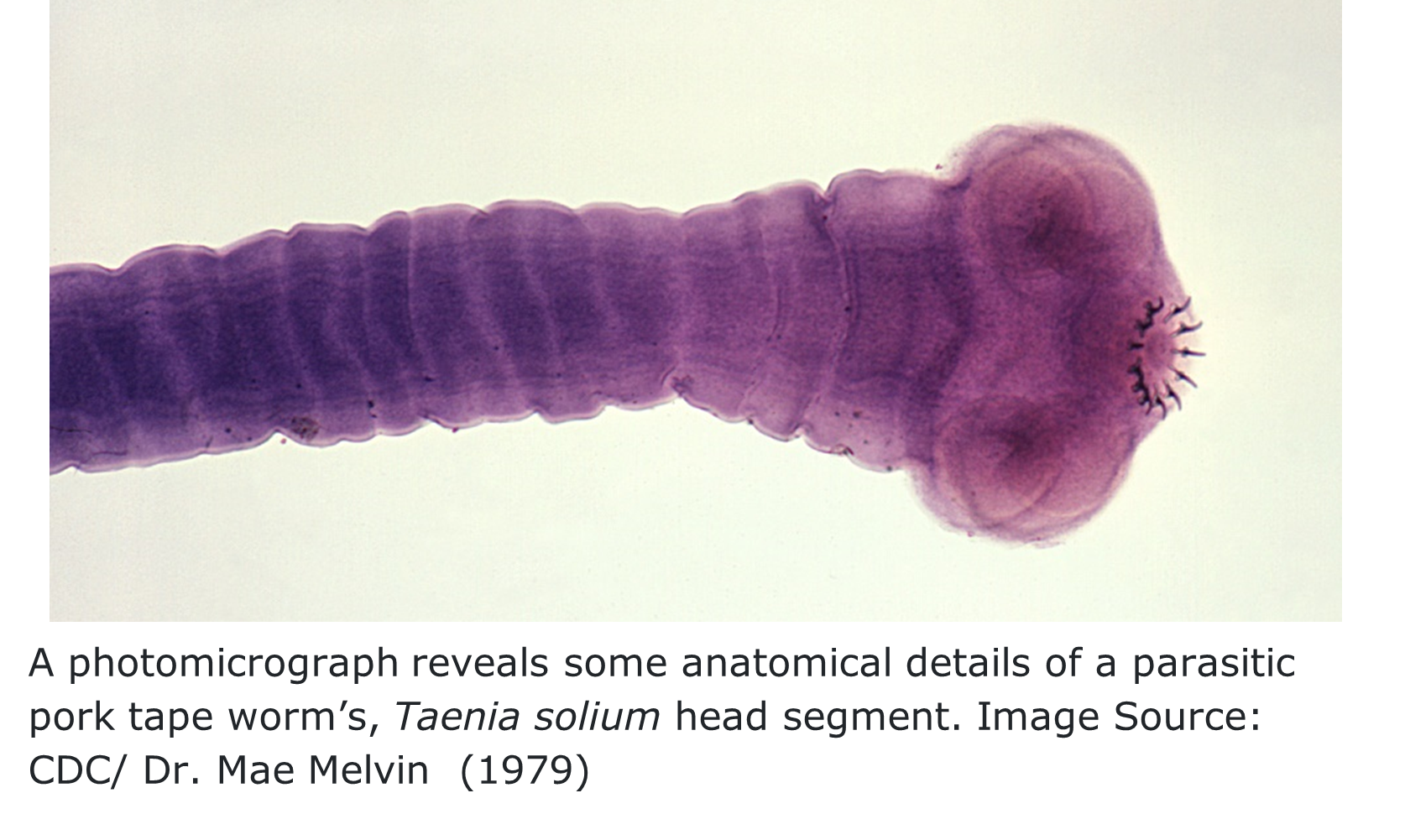
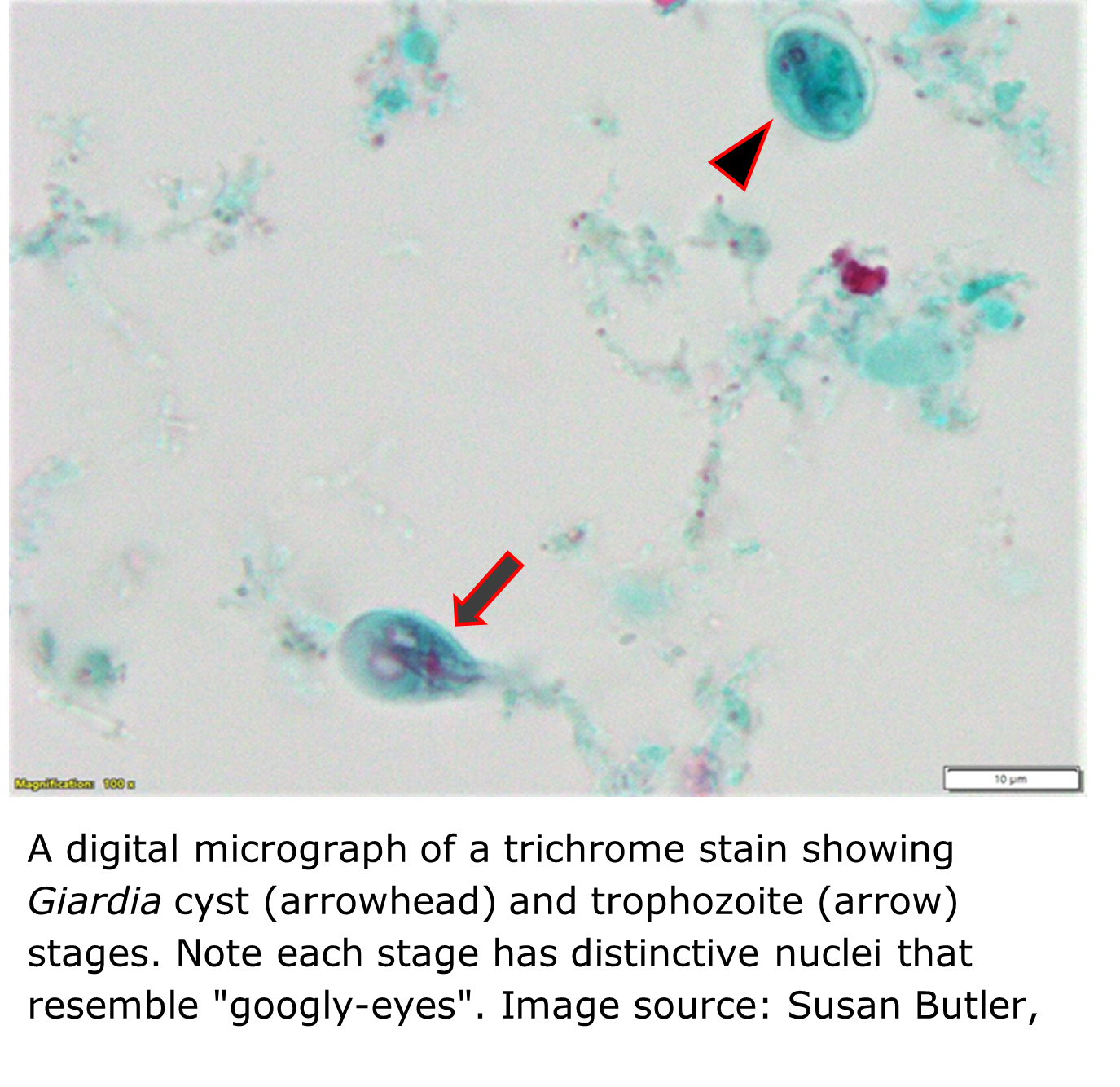
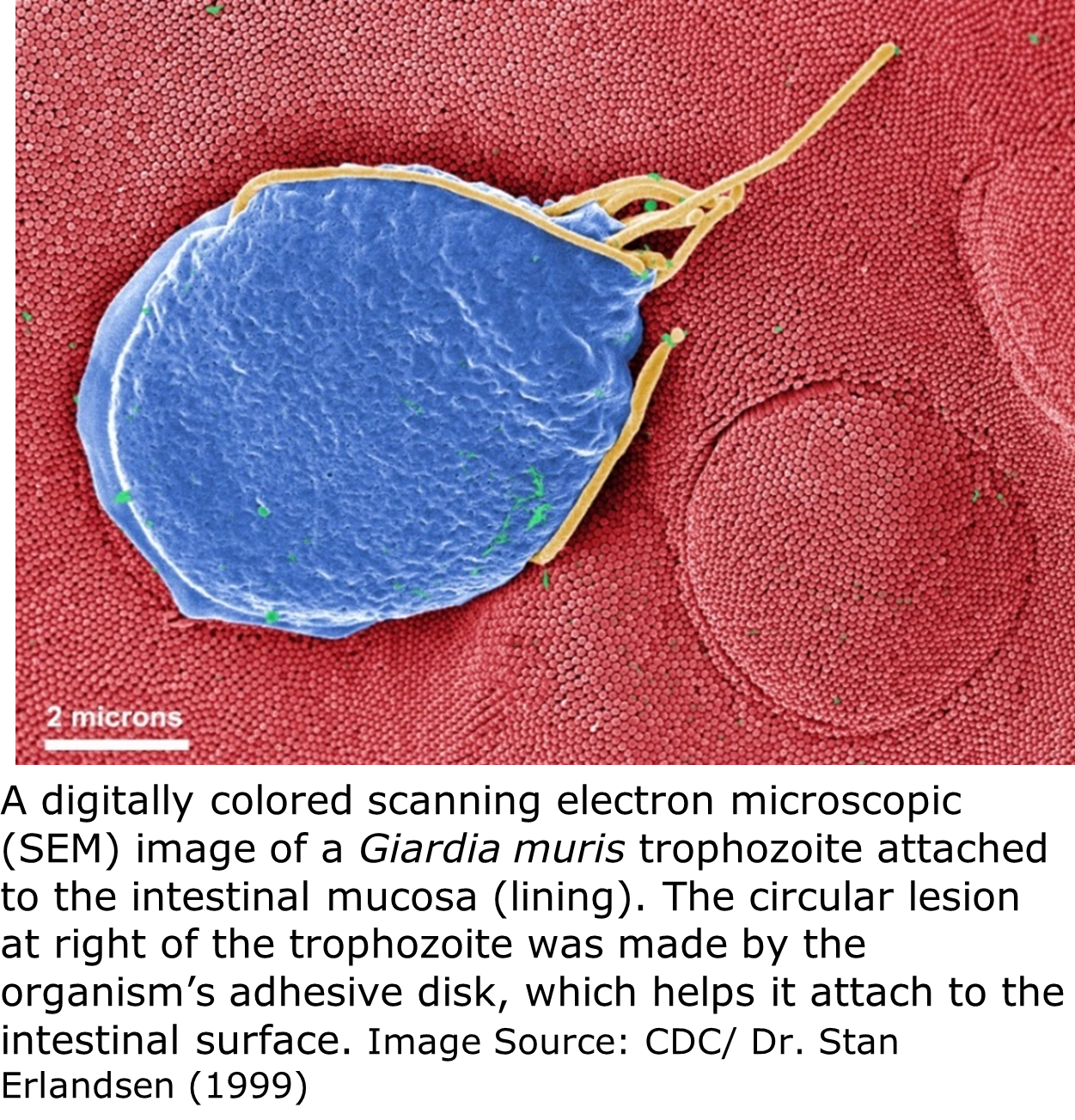
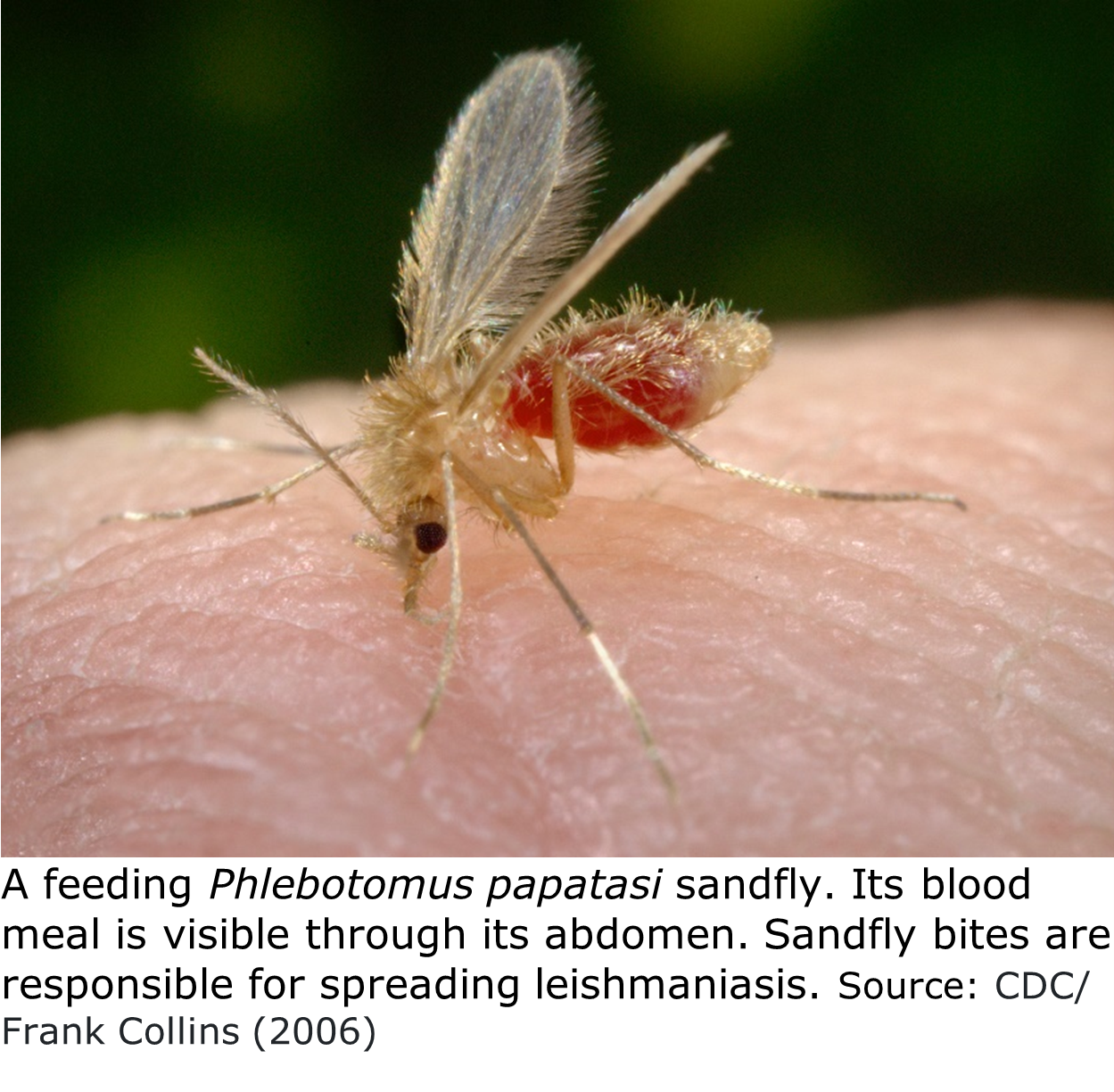
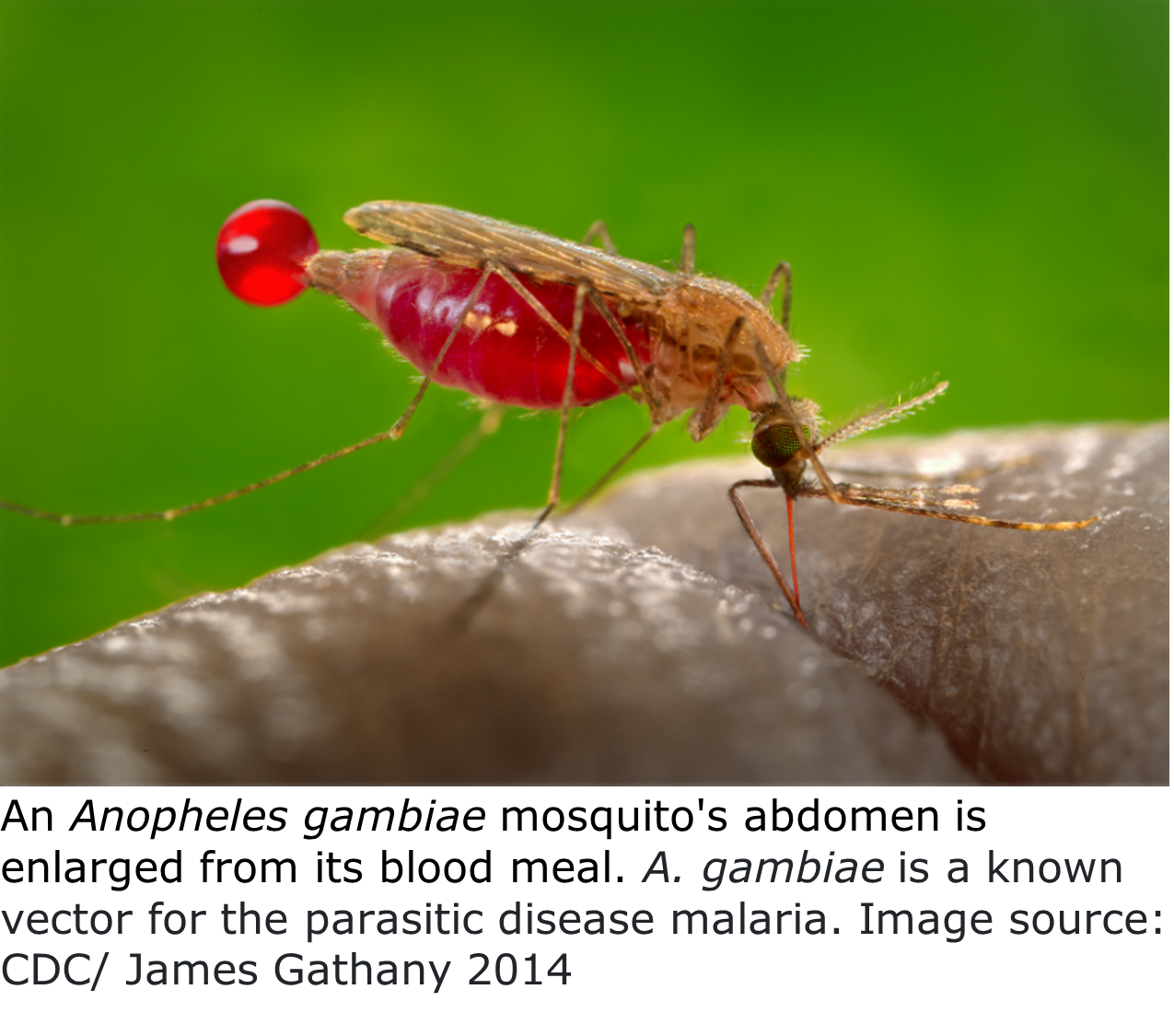
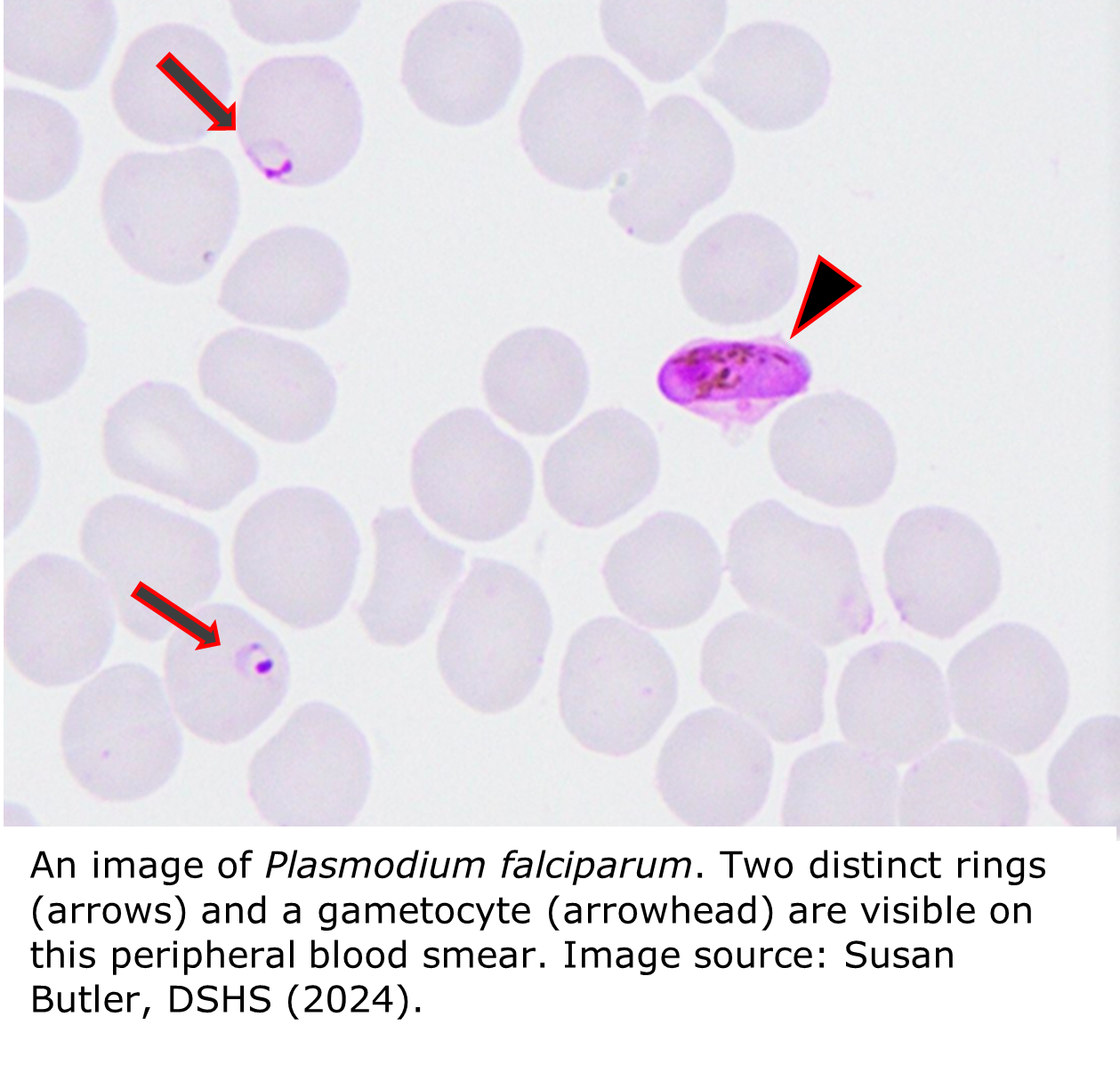
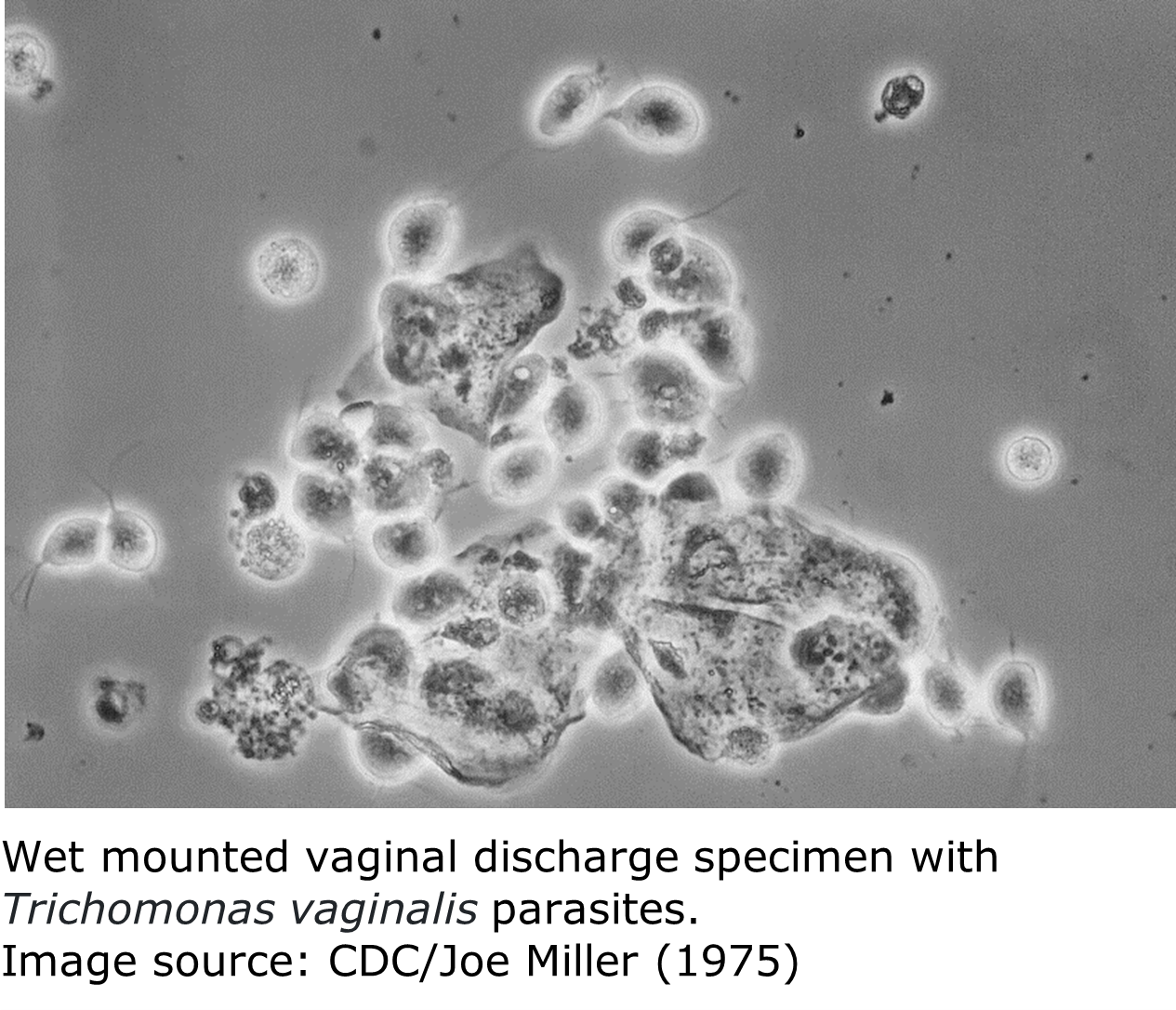
Parasites can be divided into two large groups: Protozoa and Helminths (worms). Both protozoa and helminths can be free-living or parasitic. Transmission of protozoa and helminths that infect the intestines typically happens via the fecal-oral route (when food or water contaminated by feces is ingested). Protozoa that infect the blood or other human tissues are usually spread by biting insects such as mosquitos, kissing bugs, and sandflies.
The DSHS Parasitology Laboratory tests for and identifies several medically important parasites, some of which must be reported to local and regional health departments. In such cases, the disease reporting contact, typically an epidemiologist, of the patient’s county of residence must be notified of the confirmed positive case.
A list of Texas notifiable conditions is at IDPS | Notifiable Conditions (state.tx.us). You may also scan the QR code for the list.
Parasite Diseases of Medical Importance in Texas
Note: The inclusion of external weblinks is for informational purposes only. The links do not represent an endorsement by Texas DSHS of any goods and/or services provided by these entities. These external sites may also not be accessible to people with disabilities.